Prostatitis is an inflammation of the prostate gland that is very common these days.
The prostate gland is a male organ, and therefore the disease is completely male.
Why do you need a prostate? The prostate gland is responsible for the following functions:
- the bladder forms the fluid part of the sperm with the muscles of the neck;
- produces the internal sphincter;
- dihydrotestosterone produces testosterone.
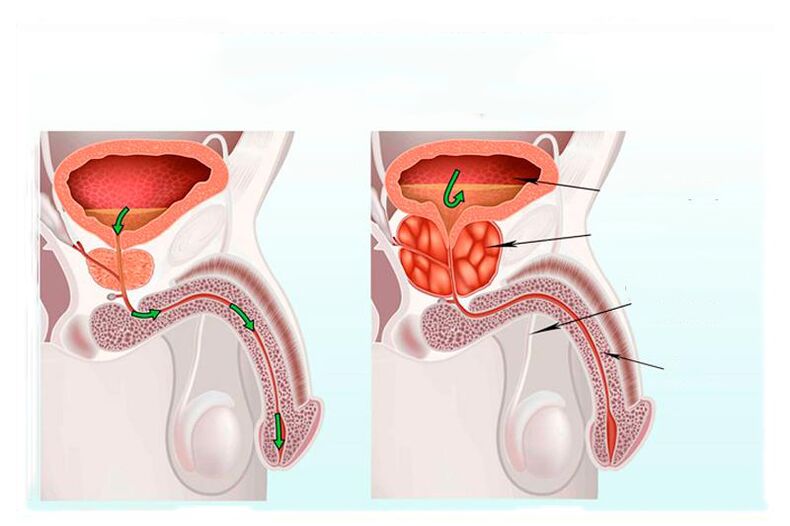
The prostate gland, or simply the prostate gland, passes through the urethra, and therefore the prostate is located around the urethra. And as the prostate grows during inflammation, it compresses the urethra and makes it harder to urinate. Men over the age of forty often suffer from prostatitis, which is the result of a malfunction of the genitourinary system.
Factors contributing to the development of prostatitis:
- hypothermia;
- infectious diseases;
- alcohol and tobacco use;
- trauma and hormonal disorders;
- sedentary work;
- urinary retention.
Prostatitis is divided into several types:
- Acute bacterial prostatitis: Escherichia coli, Pseudomonas aeruginosa, Staphylococcus aureus, etc. in prostate tissues.
- Many of these bacteria are representatives of a healthy microflora and live in our skin and stomach, but enter the prostate tissue and cause inflammation. The main symptoms of acute bacterial prostatitis are nausea and pain in the groin and lower back, frequent trips to the toilet and pain during urination, intoxication of the body and decreased quality of erection, signs of blood in the urine.
- Chronic bacterial prostatitis: occurs due to damage to the genitourinary system or infection of the organs.
- Symptoms of chronic prostatitis include pain and frequent urination during urination, discomfort in the groin, blood in the semen, and a rise in body temperature of 0, 5 - 1 degrees.
Chronic bacterial prostatitis occurs as a result of lifting heavy objects with a heavy bladder, resulting in urine entering the prostate, spasms of the pelvic muscles, thus - pressure on the prostate, damage. Symptoms include pain when urinating, and only laboratory tests can tell the difference between infections.
Chronic prostatitis
Chronic prostatitis, unlike prostatitis, is a dangerous disease that carries a number of unclear questions. What is chronic prostatitis? Chronic prostatitis is a series of tissue changes in the prostate gland and functional disorders of the prostate, the presence of inflammation characterized by the activity of the male reproductive system. Chronic prostatitis is one of the leading diseases of the male reproductive system. The classification of chronic prostatitis is divided into several subtypes:
- acute bacterial prostatitis;
- chronic bacterial prostatitis;
- chronic abacterial prostatitis;
- inflammatory prostatitis with an increase in leukocytes in prostate secretions;
- non-inflammatory process without an increase in leukocytes;
- Inflammation of the prostate without accidentally detected symptoms.
An infection caused by neurovegetative disorders causes and stimulates the development of chronic prostatitis. Hemodynamic diseases cause a decrease in immunity as a result of autoimmune and biochemical processes. Factors in the development of chronic prostatitis, infection of the genitourinary system, frequent hypothermia and sedentary work, irregular sex life or lifestyle features that lead to the constant presence of a urethral catheter are also dangerous. Important and dangerous pathogens of the disease will be disorders of the immune system, cytokines, bacteria of low molecular weight polypeptide nature that affect the functional activity of immune cells.
One of the main reasons for the development of non-inflammatory forms of chronic prostatitis is dysfunction of the pelvic floor.
Symptoms of chronic prostatitis
Symptoms include chronic prostatitis, pain and discomfort, urinary incontinence, and sexual dysfunction. Pain in the pelvic region, perineum and groin. Pain is often observed in the anus and scrotum. Sex life is disrupted and libido is reduced, but these symptoms are not observed in all patients. Chronic prostatitis alternates in nature, the symptoms worsen, and then suffocate. In general, the symptoms of chronic prostatitis are similar to the stages of the inflammatory process. Pain in the scrotum and groin is characteristic of the exudative stage, as well as frequent urination, ejaculation and painful erections. The alternate stage is not observed with pain during erection with pain in the suprapubic part, normal urination and rapid ejaculation of sperm. We can also see an increase in urine during the proliferative stage, and the process of ejaculation is somewhat delayed. In the stage of prostate sclerosis, in addition to cicatricial changes, the patient has pain in the suprapubic part, frequent urination, and sperm discharge is delayed or absent. We must not forget that the stages and disorders described above are not always visible and are not for everyone.
Given that the disease is often asymptomatic, a series of tests and laboratory tests will help to diagnose chronic prostatitis. Tests are also important to help your doctor determine the intensity of symptoms, pain, and urinary incontinence. Laboratory examination of chronic prostatitis helps to diagnose chronic prostatitis and possible infection of the prostate with atypical bacteria and fungal flora and viruses. If there is no bacterial growth in prostate secretions with increased leukocyte count, analysis for chlamydia should be performed. Microscopic examination helps to detect the number of leukocytes and mucus, Trichomonas and epithelium in the urine. The secretion obtained after prostate massage is taken for bacteriological examination and the results determine the nature of the disease. It is also important to conduct an immunological study, the results of which will help determine the stage of the disease and monitor the effect of treatment. Instrumental examination of chronic prostatitis helps to determine the stage and form of the disease with more observation during treatment. Ultrasound examination allows to study the size and volume of the prostate, the structure of the cyst and sclerotic changes in the body, the degree of enlargement and the density of the composition of the seminal vesicles. Muscle and pelvic floor myography and information on suspected neurogenic urinary disorders. An X-ray is performed to determine the initial cause of chronic prostatitis and the course of subsequent treatment. Computed tomography of the pelvic organs is performed to rule out pathological changes in the spine and pelvic organs. Diagnosis as a way to rule out a disease that is not suitable for symptoms helps to determine the nature of the pathological process: with inflammatory processes in other organs; with diseases of the rectum; with sexual disorders; with neuropsychiatric disorders such as depression or reflex sympathetic dystrophy.
Treatment of chronic prostatitis
Treatment of chronic prostatitis should be consistent and comprehensive. First, the patient needs to change his normal life and way of thinking. Eliminate the effects of harmful factors such as smoking and alcohol consumption, hypothermia. Thus, we stop the further development of the disease and soon lead to improvement. Even in preparation for treatment, dietary compliance and sexuality play an important role. The next major course in the treatment of the disease is the use of drugs. Such a correct approach to the treatment of chronic prostatitis will not only help to fight the disease, but also increase the effectiveness of treatment at each stage of prostatitis development. Chronic prostatitis generally does not require hospitalization, but in cases of severe chronic prostatitis, inpatient treatment is more useful and more effective than outpatient treatment. Drug treatment leads to good blood circulation in the pelvic organs, normalizes hormones and the immune system. In such cases, antibacterial drugs and immunomodulators, vasodilators and prostate massage are used. The use of antibacterial drugs is the basis for the treatment of chronic prostatitis. Unfortunately, the effectiveness of this therapy has been proven, but not for all types of prostatitis. Antibacterial treatment is effective in chronic bacterial prostatitis, empirical antibacterial treatment is used in chronic bacterial prostatitis.
At present, local physical therapy is very important. Physiotherapy with laser, mud and electrophoresis is the most effective. Electromagnetic radiation is based on anti-congestive and bacteriostatic action. Low-energy laser therapy stimulates microcirculation in prostate tissue, and laser therapy also has a biostimulating effect. In the absence of contraindications, therapeutic prostate massages are used.
Because the disease is affecting more and more young men, surgery is increasingly being used to treat prostatitis. One indication for surgery may be sclerosis of the seminal tubercle; Such patients often consult a doctor with no sexual feelings and signs of ejaculation. In such cases, resection of seminal tuberculosis is performed. In addition, surgery is used for sclerosis of the bladder and prostate gland.
Symptoms of prostatitis
Men who suffer from prostatitis often complain of fever and fever, and even if the temperature measured under the arm is normal, the temperature in the anus will often rise. Pain in the lower back, lower abdomen, perineum, anus and scrotum is also a signal to go to the doctor. More often during urination, there is a feeling of cramping and burning when urinating. There is a violation of the general condition, weakness, pain in the muscles and bones, severe headache.
In men, urinary incontinence is difficult with inflammation of the prostate gland, which is often accompanied by urinary retention. Constipation due to compression of the rectum by an enlarged gland is characteristic of the disease.
Treatment of prostatitis
You need to be sure of the diagnosis before starting treatment. The minimum manipulations to be performed will also require measurement of anus temperature, diagnosis and palpation of the inguinal perineum of the lymph nodes, general clinical blood test, and general urine test. It is also necessary to remove rods from the urethra and perform bacterioscopy of urine and sediment. In addition, a transrectal ultrasound examination of the prostate gland is performed.
The temperature in the anus generally rises and differs by about one degree from the temperature of the regimes with the mouse. Leukocyte count was exceeded in the urine test. Blood tests also highlight some changes, such as a decrease in the number of eosinophils and the appearance of neutrophilic leukocytosis. In immunosuppressed patients, sepsis is often accompanied by prostatitis complications.
On palpation of the perineum, the patient has pain, the patient has an increase in the inguinal lymph nodes. The prostate gland enlarges on palpation, swells and becomes hot to the touch, sometimes with heterogeneous inflammatory seals. If the prostate is inflamed, a biopsy is not performed and the infection can spread further.
Treatment of prostatitis involves the use of antibiotics against the microorganisms that cause the disease. Antipyretic drugs are also prescribed for the use of emollient laxatives to lower body temperature and facilitate bowel movements. The patient is prescribed a course of massage, which consists of squeezing the inflammatory secretion with the fingers, squeezing the ducts and, consequently, the urethra. Prostate massage improves blood circulation and has a good effect on the muscle tone of the prostate.
Prevention of prostatitis
First of all, to prevent prostatitis, you should limit yourself to food and follow a special diet. You should include foods such as parsley, asparagus, strawberries in your diet, and include pasta, etc. If you want, then there must be tough types. You should also exclude bad habits and alcoholic, spicy foods. It is very important to rule out sex as the disease progresses.
In order to prevent prostatitis from occurring, it is necessary to exclude all risk factors, ie: to follow a proper diet, to exclude bad habits and to have a regular sex life, because it does not allow sperm to accumulate. Every young man should know that sexual immorality is harmful to the prostate gland. Active sexual life increases the risk of sexually transmitted diseases. Use contraception already. Monitor your bowels and go to the toilet regularly. Another important point is work: if sedentary is connected in a way, you need physical activity, jogging is also comfortable, suitable for swimming and tennis. And do not forget the daily walks in the fresh air, it is very useful for the whole body. Hypothermia adversely affects the immune system, and this is when the infection develops. Although there are no preconditions for this, you should be examined by a urologist.
Timely treatment of any urogenital infection will help eliminate the cause of the development of prostatitis.
Folk remedies for the prevention of prostatitis are also popular, based on which recipes such as honey, nuts and dried fruits, rich in vitamins and minerals, are included in the diet. Pumpkin seeds and onions, oatmeal and seafood, liver and apples are rich in zinc and therefore have a special, important value and great benefits for the prostate gland. Add to the above tips: Empty your stomach completely and avoid constipation. This will help products such as kefir, vegetable oil and vegetable fiber. Separately, the benefits of exercise for intimate muscles should be noted.
Exercises to prevent prostatitis are easy and do not require special adaptation, they can be done anytime, anywhere. Here are some examples: Perform perineum movements as you draw in the rectum; tense the muscles of the perineum, try to stop urination, keep them in this position for as long as possible; while lying down, lift the pelvis and hold for twenty to thirty seconds, repeating these movements until the bud feels pain and fatigue. These simple exercises will be just a plus for your body.



























